This article is about plantar heel pain (plantar fasciitis). Its main aim to is to provide information and advice about the condition with an emphasis on self-help. The information is also provided in video format below.
The article is written on the assumption that the reader has been diagnosed with plantar heel pain by a health care professional. If you haven't been diagnosed but you think you might have the condition then its best to get checked out first as there are other conditions that can cause similar symptoms.
The article address plantar heel pain by answering the 3 most common questions that people ask after they have been diagnosed.
1) What is Plantar Heel Pain ?
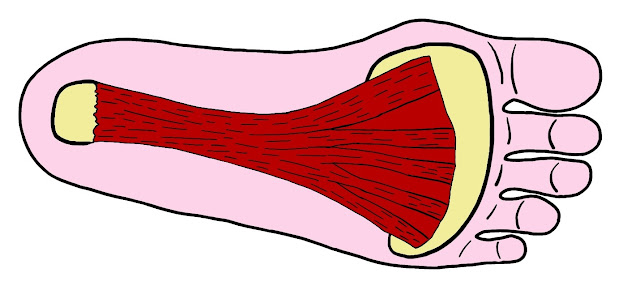 |
| The Plantar Fascia |
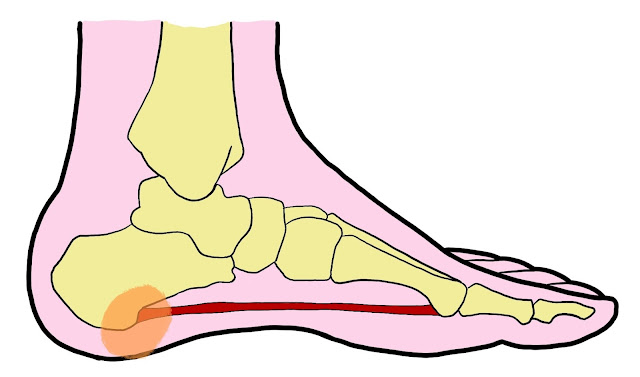 |
| Plantar Heel Pain |
The main symptom of plantar heel pain is pain in the region of the heel that takes the most body weight. It's usually quite sore to touch but as it's a deep tissue, you might have to press firmly in order to feel any tenderness. The pain is always worse when your weight is going through your heel, so usually when standing, walking or running. It's often at its worst after rest and particularly first thing in the morning when you first put your foot on the floor, and it can take a good few minutes to settle down, but then is typically painful throughout the day depending on how much time you spend on your feet. Resting with your foot off the floor is usually the most comfortable position.
A Word on Heel Spurs
Many people with plantar heel pain will be sent for an X-ray. This can be helpful in ruling out other causes of ankle region pain but is not necessary in order to diagnose this condition. However, on occasion, X-rays will identify a 'plantar heel spur', which can cause some confusion to the patient as logic would seem to suggest that a bony spur on the heel bone must be a cause of their heel pain.
 |
| image from orthoinfo.aaos.org |
The truth is though, that heel spurs are a common finding on X-rays, and are often seen in people with no heel pain at all. They tend to occur at the point where the plantar fascia attaches to the front of the heel bone and are essentially a calcification of that attachment point.
The spur is simply a legacy sign that the plantar fascia may have been irritated at some point in the past, often many years ago. It is basically an effect of the condition (in some people) but it is not a cause of it. In fact, heel spurs rarely occur on the part of the heel that contacts the floor, as you can see on the X-ray above. So, in the vast majority of people, heel spurs seen on X-ray are completely irrelevant and of no concern. Only the very large spurs that occur on the weight bearing part of the heel bone will ever require surgical treatment.
2) Why have I got it ?
Well the first thing to say is that you are by no means alone. This is unfortunately a very common condition, particularly in the 40-60 age group. It accounts for between 11 and 15% of all foot complains to health care professionals, and it occurs in about 8-10% of regular runners. It's slightly more common in females and people who have repetitive and manual occupations where they stand a lot. It's not just runners and manual workers though. A recent UK based study found almost 10% of the general over 50's population had some symptoms of plantar heel pain. So as you can see, it's a very common problem.
Plantar heel pain is essentially an overuse condition. It's caused when the plantar fascia becomes overloaded to the point where its collagen fibres begin to degenerate. And it's really important to understand this if you want help settle down the symptoms. Plantar heel pain is caused because you are exceeding the capabilities of your plantar fascia. Basically, you are doing more walking, running or standing than your plantar fascia can cope with. And what it can cope with is mainly determined by your lifestyle and your foot posture.
The 2 biggest risk factors for developing the condition are an inactive lifestyle and being overweight. It's also seen more often in people with certain foot postures, particularly a low plantar arch, which can put extra strain on the plantar fascia and make it more vulnerable to developing the condition.
 |
| A Low Arch |
It's also more common with conditions like diabetes which is known to affect collagen health, particularly if isn't well controlled.
Having an unhealthy plantar fascia and then suddenly starting to do more walking or standing than it can cope with, is the single most common reason for developing the condition.
However you may not have any of those risk factors and have a perfectly healthy Plantar Fascia but you're just overloading it with activities beyond your usual level. For example you might have taken up running and have increased your distances too quickly for your Plantar Fascia to adapt. Pushing a new sport too far and too fast is the next most common reason for developing the condition.
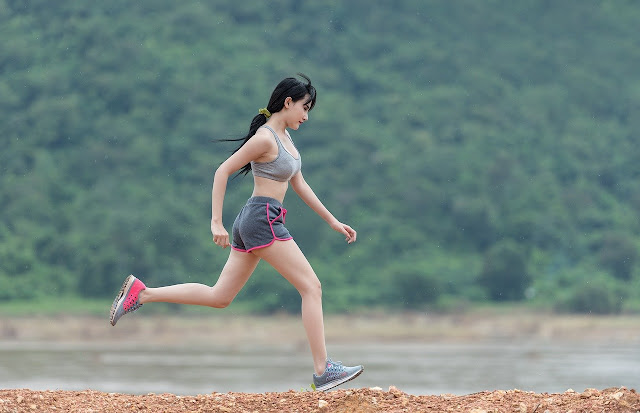 |
| Overactivity causes Plantar Heel Pain |
3) What can I do about it ?
In a nutshell, there is good news and bad news. The good news is that it will usually get better by itself in the majority of cases, the bad news is that it can take a long time. 1-2 years is not unusual.
Unfortunately, despite what you might see online, there is no quick fix and no reliable treatment that works for everyone. In fact if you google 'treatments for plantar fasciitis' you will find a myriad of different suggestions which should ring alarm bells that we don't really have a good reliable treatment that works for everyone. And this can obviously cause much confusion, wasted time and wasted money.
The best evidence we have comes from clinical research, and a large study published in 2021 has collected the best available evidence from published research, the opinions of 14 experts and also 40 patients with the condition and they have come up with a consensus of the 5 most useful self help treatment options for plantar heel pain. And these are :-
i) Managing load
Now it might sound obvious but this was found to be the single most effective way of reducing symptoms. Remember that the cause of plantar heel pain is overloading of the plantar fascia. Well, in order to get it better, we have to reduce the load and give the plantar fascia a period of relative rest. Only then, can we give it a chance to go through a healing process.
But what is relative rest? Well it isn't total rest from walking and general weight bearing. It's a general reduction in the activities that are causing the pain. Whether that's standing, walking or running. And you have to reduce these activities to the degree where the pain starts to improve. This will be different for different people but as a general rule, you should be reducing your weight bearing activities until the pain becomes mild and manageable while doing that activity, and the pain doesn't worsen again the next day.
If you still get a lot of discomfort while standing or walking and it feels worse the next day then you are still doing too much and you are still aggravating the condition. This may take a bit of experimentation but its really vital that you stop aggravating the plantar fascia or you're going to be fighting a losing battle. A step counter or smart watch can be really helpful in giving you some feedback about how much time you are spending on your feet and you can then relate this to your symptoms in order to find out what you can manage, and more importantly what is too much for you.
A Word on Running
If you are a runner, then the same advice applies. You are going to need to slowly reduce your mileage until the pain is minimal & manageable and is does not worsen the next morning. If you have a heavy heel strike, then an adjustment in your running style, so you take more weight through the forefoot and less weight through the heels might be beneficial. If you still can't reduce your mileage enough to reduce the pain, then you will need to stop running completely for a period of time (at least 6 weeks) and then start again slowly.
ii) General Footwear
The next think to consider is general footwear. The researchers found that walking barefoot or in flat unsupportive shoes such as flip flops or converse type shoes aggravated the condition, while more supportive shoes, typically well-fitted trainers were the most comfortable.
iii) Taping
The next self-help treatment found to be useful by the researchers was taping. Applying a rigid sports tape in a way that supports the plantar arch was found to help reduce pain in the short term. Many different techniques have been described but perhaps the most commonly used is the 'low dye taping technique'. However, taping is time consuming and can be awkward to apply yourself and so you might be best moving straight to treatment 4.
iv) Supportive Insoles
Insoles are easier to use and do a better long term job of supporting and cushioning the foot than taping. There are 2 main types of insoles for plantar heel pain. The first are the gel heel pressure relief inserts that essentially spread the pressure over the heel and reduce pain when standing and walking.
 |
| Gel Heel Insoles |
 |
| Arch Support Insoles |
You can also find insoles that do both jobs. The main thing is that they should be comfortable and certainly not increase the pain. If you struggle to find something that suits your foot posture then you could consider seeing a podiatrist for custom fit insoles that are moulded to your specific foot posture.
 |
| A Podiatrist can make custom fit insoles |
Whatever insoles you use, you should wear them pretty much all the time when on your feet. Move them from shoe to shoe as needed, or buy a few pairs. I say pairs, as even though your other foot may be perfectly fine, it's best to use insoles for both feet so not to throw you off balance.
v) Stretches & Exercises
The last self-help treatment supported by research are the exercises and stretches. Stretches are often advised for plantar heel pain but whilst they can make you feel better for a short time, they don't tend to do much else. When combined with strengthening exercises though, they can be much more effective. You should only start exercising when the pain is under some control by managing your load as discussed earlier.
There is no point in exercising a highly irritable plantar fascia when it really needs rest instead. Allow it to calm down with the other treatments mentioned earlier. The key is that they should always be fairly comfortable. You certainly shouldn't be wincing with pain as you do them, and any discomfort should settle down quickly. I've made a video to demonstrate a suitable stretch and exercise programme which you can see below.
Night Splints
Another pain relief option which wasn't covered in this paper but which other studies have found can be helpful for that early morning pain, are the night splints. The reason why plantar heel pain is worse in the morning is because the plantar fascia shortens overnight when the foot is relaxed, and then it stretches abruptly when you first put weight through it again. So a splint to lift the foot up and keep the plantar fascia on a bit of stretch is usually helpful in reducing that morning pain.
There are 2 general types available. The ones which pull your foot up and the ones which support the foot from underneath. They don't work for everyone but if morning pain is a particular problem for you then its worth giving them a go as they are fairly inexpensive.
 |
| A Night Splint |
Immobilisation Boot
Lastly, if you just can't reduce your weight bearing activities enough, or your heel pain is really severe & irritable, and causing you to limp, then I would recommend an immobilisation boot. This is usually fitted by a Health Care Professional but you can buy them online and I'll put a link below.
 |
| A typical Immobilisation Boot - Amazon Link |
An immobilisation boot will prevent all foot and ankle movement and therefore offload the plantar fascia as much as possible. They need to be worn for at least 6 weeks and sometimes longer. They come off at night and when driving but stay on pretty much all the time otherwise. They are commonly used with Achilles tendon injuries so you've probably seen people using them. They look like a ski boot. They are a bit cumbersome at first but you do get used to them and they are very effective at reducing the pain. After 6 weeks use, if the pain has settled, then you can start to slowly increase your activity levels along the lines previously discussed. If the pain has not settled, then a further 6 weeks use may be needed.
That completes the self-help section. Any other self-help treatments that you see online are not supported by the evidence, at least as of Dec 2021, so don't waste your time or money. Also, ignore the silly click bait articles and videos that claim to cure plantar heel pain in a week or other such nonsense. If your plantar heel pain gets better in a week, then it wasn't plantar heel pain.
What if my Plantar Fascia ruptures (tears)
If you've had plantar heel pain for a while and you experience a sudden increase in pain associated with a sudden 'tearing' sensation on the heel, and then perhaps some local swelling or bruising, then you might have torn or at least partially torn your plantar fascia. An ultrasound or MRI scan can confirm the diagnosis. A plantar fascia rupture or partial tear is usually treated with 6-12 weeks of complete rest in one of the immobilisation boots previously discussed. The plantar fascia will usually heel itself over this time as long is has an appropriate period of rest.
_________________________________________________________
If you are really struggling with plantar heel pain, and haven't had a great response to the self-help treatments we've discussed then the rest of this article talks about some of the other evidence based treatments available. They are certainly not a guaranteed cure and you'll need to discuss your individual case with a clinician specialising in foot and ankle conditions.
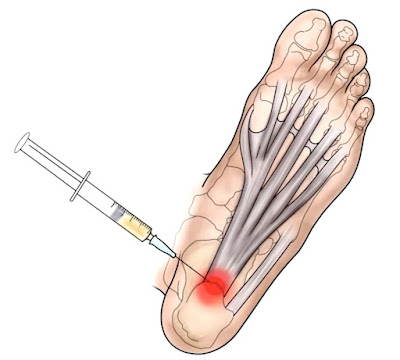
This was a commonly used treatment for plantar heel pain but has fallen out of favour over recent years as the evidence has shown it is not quite as helpful as we first thought, and indeed can be potentially harmful. We do know that cortisone can work well in short term but sometimes the pain will return in a few weeks or months and the patient then comes back asking for another.
And this is where the problems arise because we now know that with each repeated injection, there is an increased risk of causing long term weakness of those collagen fibres which can then cause the plantar fascia to completely rupture or it can cause thinning and weakness of the plantar fascia that ultimately prolongs the condition, causing exactly the opposite effect to what we want with treatment.
As a result, I am cautious about providing injections and if I do, it’s usually a one-off treatment for patients who are really struggling. I always inject the plantar fascia using ultrasound image guidance in order to ensure the drug is delivered accurately into the target area. Image guided injections also help to minimise pain and prevent complications.
The other treatments I'm going to talk about all work on the premise that plantar heel pain can be considered a type of injury where the healing process becomes stuck, and by trying to re-injure the plantar fascia in a controlled way, we try to kick-start this healing process and stimulate recovery of the degenerative collagen fibres.
The first of these 'provocative treatments' is 'Extra Corporeal Shock Wave Therapy'. This is a treatment which uses high pressure sound waves to disrupt the collagen fibres in a way that stimulates a healing response. It's a treatment that usually last around 10 minutes and is typically delivered once a week over a 3 week period. It can cause a temporary increase in pain as it is essentially re-injuring the plantar fascia in order to prod it into kick-starting the healing process. Patients are then reviewed about 6 weeks later when the treatment can be repeated if needed.
 |
| Shock Wave Therapy |
Needle Fenestration / Dry Needling
Another way of trying to stimulate this healing response in to cause some bleeding around the plantar fascia. We know that blood contains various growth and repair factors that initiate healing when you have injury. By high-jacking this system we can try to encourage the plantar fascia to repair itself. The easiest way of doing this is by using a needle to cause some disruption and local bleeding. Acupuncturists can do this in a process called 'dry needling' but it can an uncomfortable process.
 |
| Ultrasound Guided Needle Fenestration |
A better way is using some local anaesthetic and then inserting a normal hypodermic needle under ultrasound guidance directly into the painful part of the plantar fascia. The needle tip is then used like a mini scalpel in order to 'injure' the collagen fibres. We call this 'Needle Fenestration' and it's done using ultrasound guidance to ensure the needle hits the right target area. Because you are trying to cause local inflammation, you should not use anti-inflammatory medication like ibuprofen for 2 weeks before or after the procedure.
The latest treatment technique takes this process a step further. A process called PRP (platelet rich plasma) involves taking some blood from the patient, spinning it in a centrifuge and then separating out the platelets which contain all those growth and repair factors. This concentrated serum is then injected into the plantar fascia. PRP is becoming more widely available but you might struggle to find it being offered on the NHS at the moment because its still an active area of active research and the jury is still out regarding its overall effectiveness.
 |
| Platelet Rich Plasma |
Surgery
And finally, for the most severe cases that have resisted treatment and the passage of a few years, surgery is sometimes considered as a last resort option. There are a number of different procedures offered but results are quite variable and as such, most surgeons will be reluctant to operate in all but the most severe cases.
_____________________________________________________________________________
This article provides general information related to various medical conditions and their treatment. It is intended for informational purposes only and not a substitute for professional advice, diagnosis or treatment provided by a doctor or other qualified health care professional. The information provided does not constitute personal advice or guarantee of outcome and should not be used to diagnose yourself or others. You should never ignore advice provided by a health care professional because of something you have seen or read on this website. You should always consult a doctor or other qualified health care professional for personal medical advice.
This website uses affiliate links for certain products that may be illustrated in the articles. When you use one of these links to purchase a product, the site receives a small commission at no extra cost to yourself. This helps support the running costs of the website and YouTube channel.